Knowing Mesenchymal Stem Cells
Stem cells are cells with differentiation potency, typically isolated from human embryos, bone marrow, umbilical cord blood and peripheral blood. Stem cells can divide into identical cells (i.e., self-renewal), and differentiate into specialized cells exerting specific functions. They play a pivotal role in the human body, be in charge of cellular regeneration and wound healing of human tissues and organs. In response to different microenvironmental cues, stem cells can differentiate into three germ layers. Each layer consequently differentiates into specific cells forming various types of tissues and organs. According to their differentiation potency, they can be classified in three different types as follows:
| Type of Stem Cell | Origin | Differentiation Potency |
|---|---|---|
| Totipotent stem cells | Isolated from a blastomere of 16-cells that is the morula after 4 times of division of the fertilized egg | They can differentiate into all types of cells in tissues and organs. |
| Pluripotent stem cells | Isolated from the inner mass cells of the blastocyst | They can differentiate into any of the three germ layers including ectoderm, endoderm and mesoderm. Embryonic stem cells (ESC) and induced pluripotent stem cells (iPSC) are this type of cells. |
| Multipotent stem cells | Isolated from bone marrow, umbilical cord blood, adipose tissue, synovial fluid, pulp cavity and peripheral blood | They can differentiate into multiple specialised cell types present in a specific tissue and organ, but only those of related germ layers of cells. For example, mesenchymal stem cells can differentiate into cells related to mesoderm, including connective tissue, muscle, bone, circulatory system (blood vessels and heart), etc. |
Mesenchymal stem cells (MSCs) are multipotent stem cells, originating from the germ layer of the fetus at early stages. MSCs have a great capability of self-renewal and multiple differentiation potency that they can develop into neurons, bone cells, adipocytes, hepatocytes, etc. After tissue damage, MSCs can contribute to tissues repair. This can largely improve the currently incurable diseases.
In recent years, MSCs have become the most important topic in stem cell research. Moreover, their evident efficacy on anti-aging has been brought to practice. Studies have shown that the number of MSCs obtained from placenta and umbilical cord is higher compared to other sources. Previous studies of stem cell therapy showed that MSCs can significantly ameliorate diseases such as Parkinson’s disease (PD), Alzheimer's disease (AD), spinal cord injury, and liver cirrhosis, etc.

Because totipotent and pluripotent stem cells are difficult to obtain and face ethical concerns (until now no countries permits a clinical use of embryonic stem cells), MSCs, one of the multipotent stem cells, become the major material in many of basic research. MSCs possess following advantages:
- Sources: MSCs are comparably easy to harvest from many sources.
- Differentiation potency: MSCs grow fast in culture and can differentiate into multiple types of cells forming human organs and tissues, such as adipocytes, osteocytes and chondrocytes.
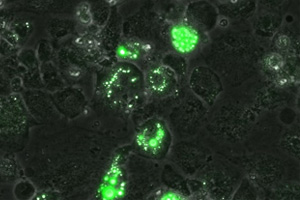
- In vitro culture: MSCs are adherent cells that can be easily plated on plastic culture dishes.
- Immunomodulation: MSCs have immunoregulatory potential and have been proven to reduce abnormal immune system activity.
- Clinical applications: The antigenicity of MSCs is much lower than other types of stem cells. Thus, clinically, MSCs can be transplanted without the need for donor-recipient matching. They hardly induce graft-versus-host disease. Hence, MSC engraftment is compatible in infants and families.

Mesenchymal Stem Cell |
Adipocytes |

Chondrocyte |

Osteocytes |
In the field of regenerative and personal medicine, MSCs are frequently used as the source of cell therapy and have been studied further including tissue engineering, mitigating graft-versus-host disease (GVHD), cell therapy and improving the effectiveness of cell therapy. These studies can be classified into four categories as follows:
- in vitro differentiation potential
Recent advances in this field indicate that MSCs can differentiate into not only endoderm-related tissues but also cell types of other germ layers via genetic modification (transcription factors) and culture conditions (growth factors). Since 2009, Naghdi’s team has successfully utilized cell culture media containing HGF and EGF to induce differentiation of MSCs into neural cells. Hang’s team overexpresses transcription factor HNF4A in MSCs to induce hepatocyte differentiation. Furthermore, therapeutic capability of these hepatocytes in repairing liver damages have been tested on animal models.
- Immune Modulation
For the purpose of MSCs being widely use in cell therapy and transplantation, understanding their immune-modulating capabilities will help advance in clinical use. Current studies indicates that MSCs can escape the attack from NK cells due to the lack in expression of MHC Class I molecules. In addition, MSCs can modulate the immunoresponses by releasing leukaemia inhibitory factors (LIF) and interferons. In conclusion, these properties of MSCs make them the first choice for cell transplantation.
- Chronic Disease Treatments
Because MSCs possess differentiation, anti-inflammatory and immune modulatory potentials, MSCs have therefore become an important cell source to treat three classes of chronic diseases:
- Neurodegenerative Disease
MSCs have been induced to differentiate into neural cells in vitro and transplanted to animals. The result showed that this treatment effectively alleviated animals' limited mobility, and increased their survival rates. Furthermore, Mazzini’s team used MSCs in animal models of amyotrophic lateral sclerosis (ALS). They found spine abnormalities have structural transformations accompanying cellular proliferation. There are same therapeutic effects in other neurodegenerative diseases, such as AD and PD. After injection of MSCs, they autonomously migrate to damaged brain areas, like hippocampus and cortex, activate the synthesis of repair enzymes and induce cellular proliferation. Consequently, MSCs alleviate the degree of cell damages and neural cells which are repaired gain normal function.
- Autoimmune Diseases
Gonzalez’s team has shown that MSCs can modulate autoimmune T cell responses by secreting IL-10 to reduce symptoms of rheumatoid arthritis. Moreover, in animal model for type I diabetes, they have observed that MSCs can differentiate into insulin-secreting cells and also reduce autoimmune attacks on ß-cells.
- Cardiovascular Diseases
Shake’s team has proven that the transplantation of MSCs in vivo can decrease the area of myocardial infarction and enhance the myocardial contractility.
- Neurodegenerative Disease
- Other related applications
One of the key factors in cell therapy is whether the transplanted cells are able to migrate to the injured area and repair it. Previous studies have found that MSCs can achieve these tasks by expressing chemokine receptor type 4 (CXCR4) and its compartment protein, stromal-derived factor (SDF).
According to the statistics of ClinicalTrials.gov, 651 cases of using MSCs in clinical applications have been registered by the end of January 2017.
| Clinical applications | Treatments |
|---|---|
| Cardiovascular disease | Direct local injection of MSCs for myocardial infarction |
| Autoimmune disease | Congenital diabetes, Rheumatoid arthritis |
| Osteoarthritis | Implantation of MSC-scaffolds |
| Liver disease | Acute and chronic hepatitis, Hepatoma, Liver cirrhosis |
| Graft-versus-host disease | Modulation of immune responses after transplant. |
| Respiratory diseases | Chronic Obstructive Pulmonary Disease |
| Kidney disease | Kidney failure |
| Muscular dystrophy | Duchenne Muscular Dystrophy |
| Skin disease | Healing of local skin lesions and sores |
| Neurodegenerative disease | Alzheimer's disease, Parkinson’s disease |
| Cancer related treatment | Conjugate MSCs with anticancer drug to suppress tumor metastasis through immune modularity and homing tendency to tumor of MSCs. |
Successful cases in clinical applications
An FDA-approved human bone marrow-derived MSC product Prochymal (Osiris Ltd.), used in patients ,such as lymphoma and leukemia patients to prevent graft-versus-host diseases (GvHD), was launched on 20th of December, 2005. MSCs regulates the immune responses including the concentration of anti-inflammatory cytokines and the activity of T cells to enhence the recovery rate. To sum up recent studies and successful cases, it indicates that mesenchymal stem cell is a novel clinical tool. By the aid of more studies in the future, MSCs might be a new hope for hardly curable diseases, cancer treatments, organ transplantation, and neurodegenerative diseases.